Publication highlights
-
![]()
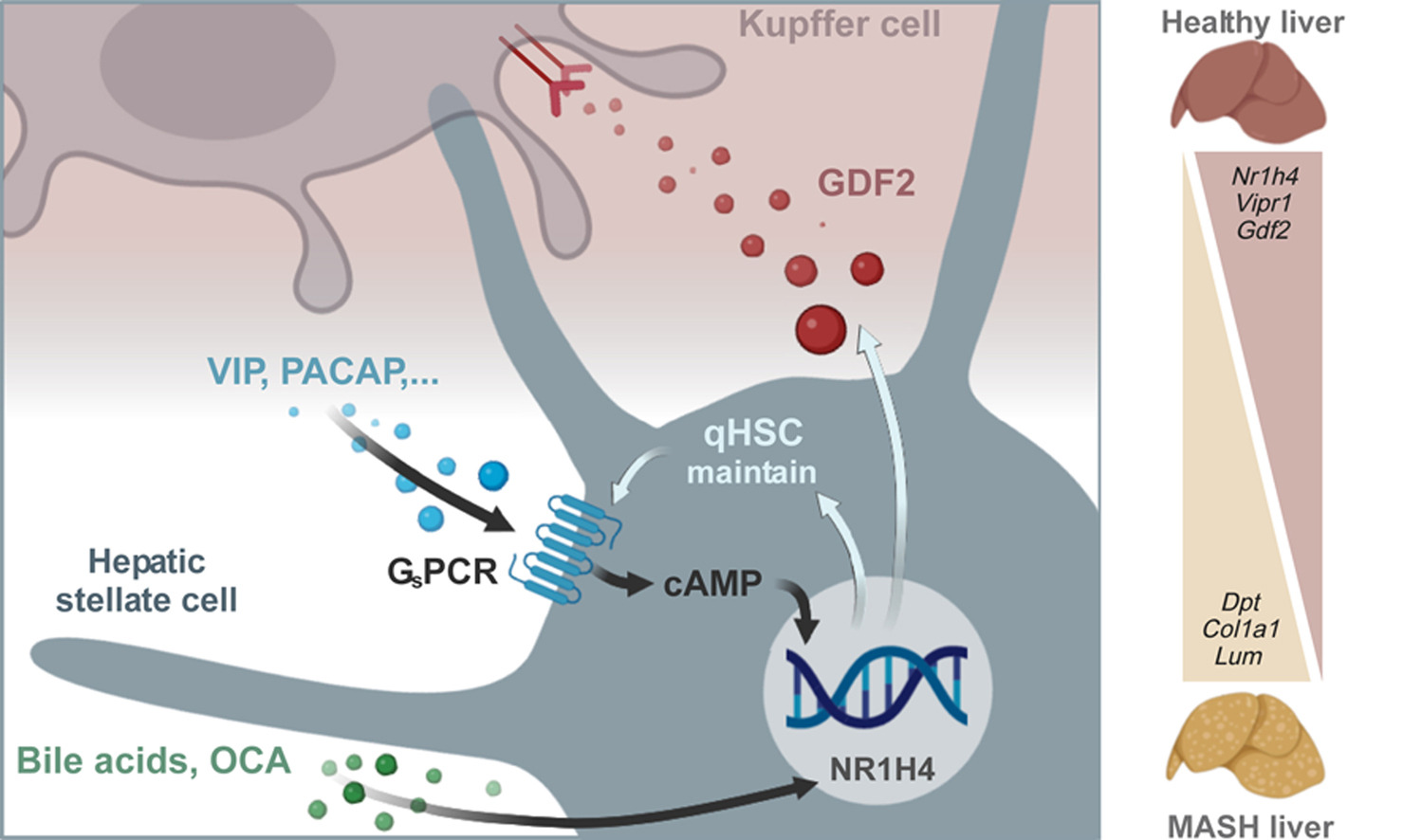
Single cell-resolved study of advanced murine MASH reveals a homeostatic pericyte signaling module
Metabolic dysfunction-associated steatohepatitis (MASH) is linked to insulin resistance and type 2 diabetes and marked by hepatic inflammation, microvascular dysfunction, and fibrosis, impairing liver function and aggravating metabolic derangements. The liver homeostatic interactions disrupted in MASH are still poorly understood. We aimed to elucidate the plasticity and changing interactions of non-parenchymal cells associated with advanced MASH.
-
![]()
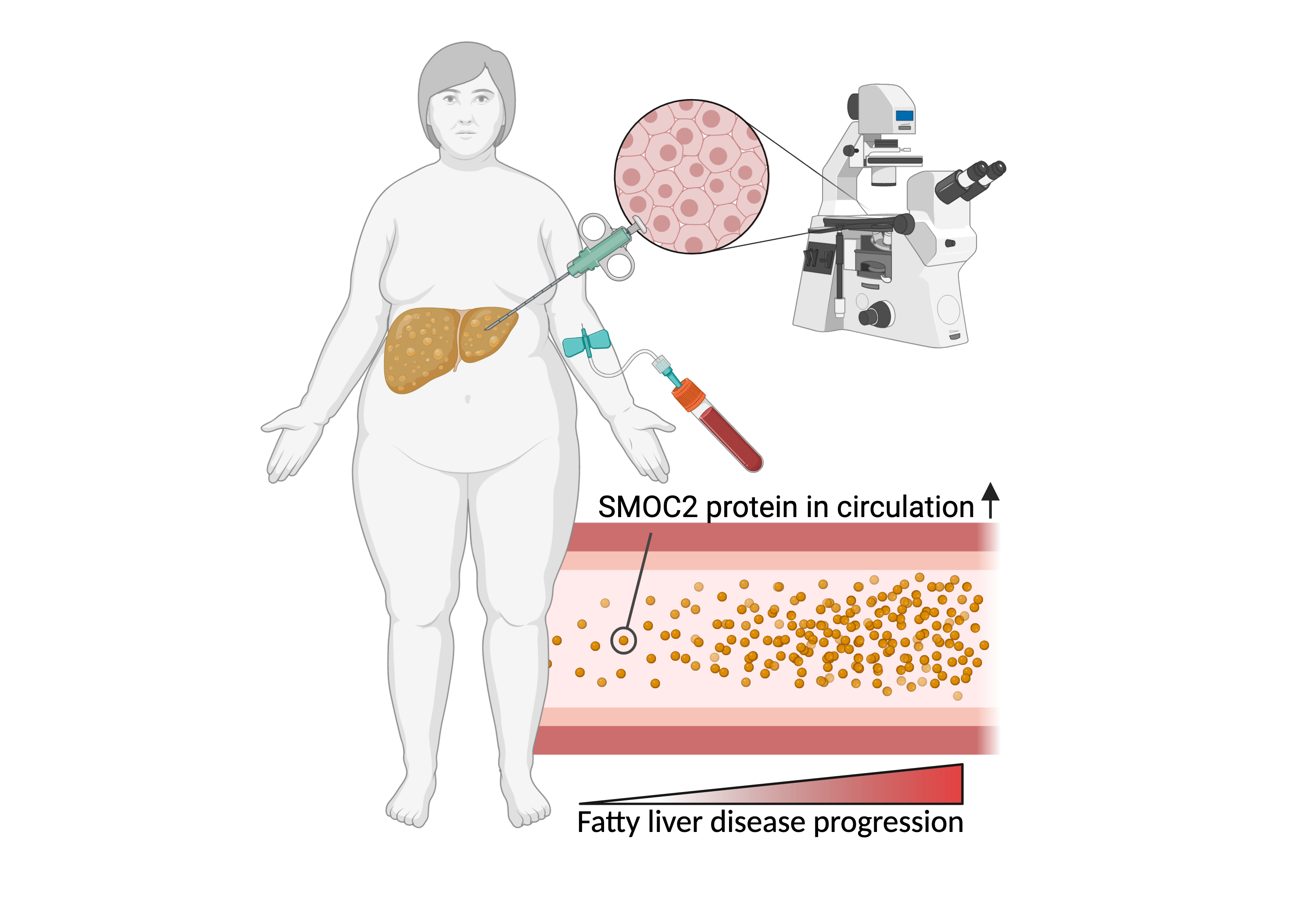
SMOC2 as a novel biomarker for non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD) and its progressive form, non-alcoholic steatohepatitis (NASH), are the most common forms of chronic liver diseases. Currently, liver biopsies are the gold standard for diagnosing NAFLD. Blood-based biomarkers to complement liver biopsies for diagnosis of NAFLD are required. We found that activated hepatic stellate cells, a cell type central to NAFLD pathogenesis, upregulate expression of the secreted protein SPARC-related modular calcium-binding protein 2 (SMOC2). SMOC2 was elevated in blood samples from patients with NASH and may hold promise as a blood-based biomarker for the diagnosis of NAFLD.
-
![]()
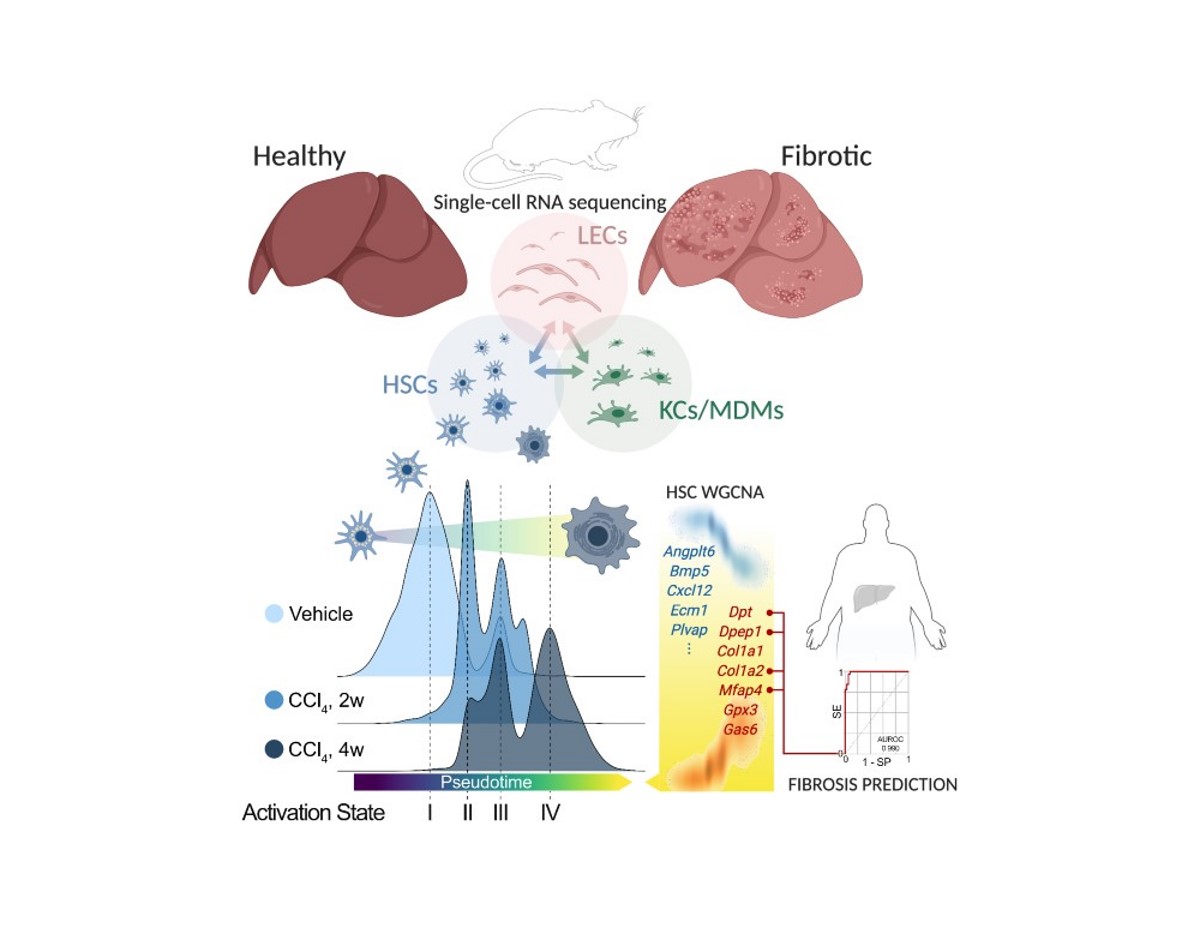
Transcriptional Dynamics of Hepatic Sinusoid-Associated Cells After Liver Injury
Non-alcoholic fatty liver disease (NAFLD) and its progressive form, non-alcoholic steatohepatitis (NASH), are the hepatic manifestations of metabolic syndrome. Histological assessment of liver biopsies is the gold standard for diagnosis of NASH. A Liver biopsy is resource heavy, can lead to complications such as bleeding, and does not fully capture tissue heterogeneity of the fibrotic liver. Therefore, non-invasive biomarkers that can reflect an integrated state of the liver are highly needed to improve diagnosis and sampling bias. Hepatic stellate cells (HSCs) are central in development of hepatic fibrosis, a hallmark of NASH. Secreted HSC-specific proteins may, therefore, reflect disease state in the NASH liver and serve as non-invasive diagnostic biomarkers. We performed RNA-sequencing on liver biopsies from a histological characterised cohort of obese patients to identify and evaluate HSC-specific genes encoding secreted proteins. Bioinformatics was used to identify potential biomarkers and their expression at single-cell resolution. We validated our findings by single-molecule fluorescence in situ hybridisation (smFISH) and ELISA to detect mRNA in liver tissue and protein levels in plasma, respectively. Hepatic expression of SPARC-related modular calcium-binding protein 2 (SMOC2) was increased in NASH compared no-NAFLD and elevated in blood samples from NASH patients and may hold promise as a blood-based biomarker for NAFLD diagnosis.
-
![]()
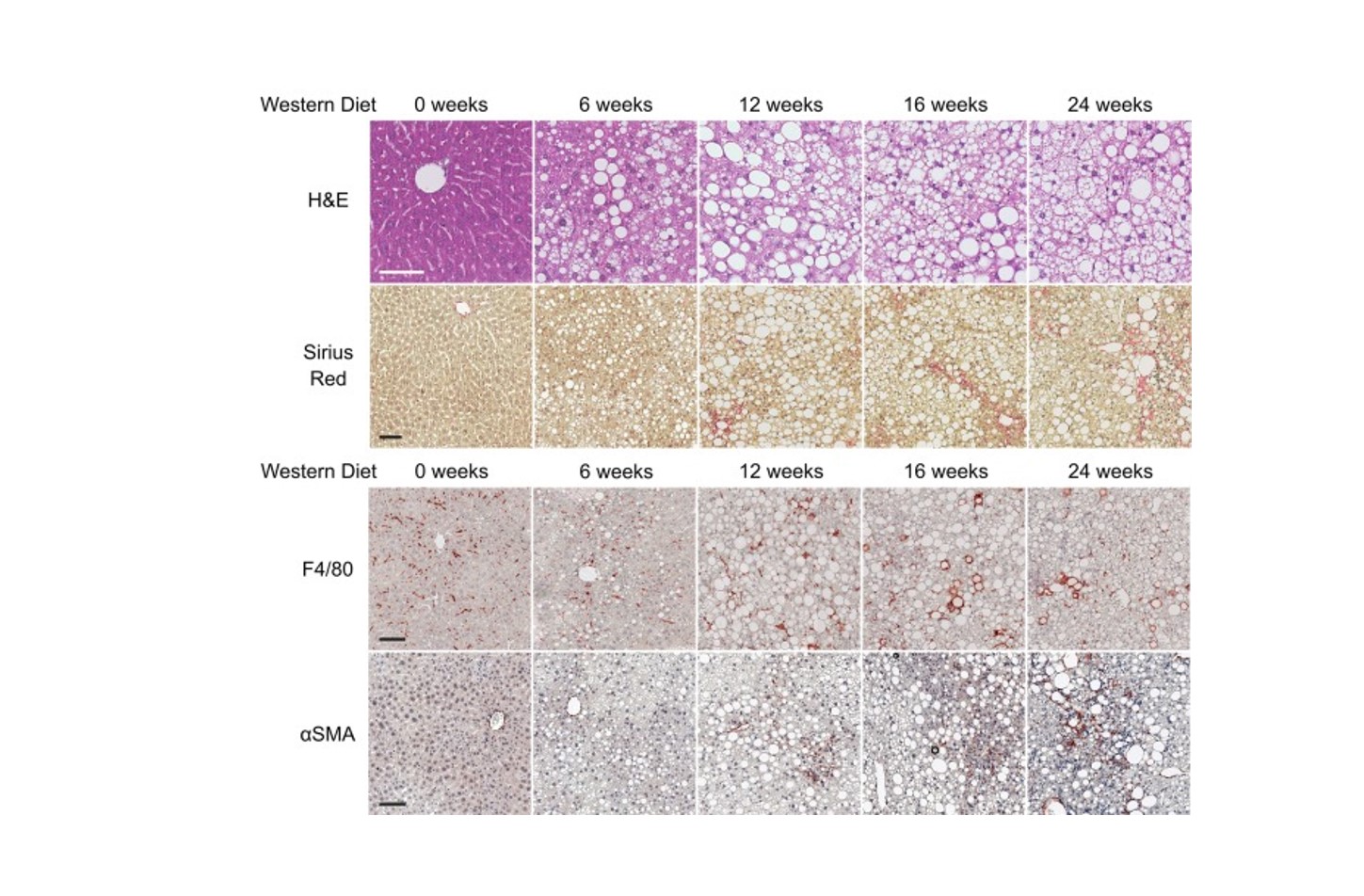
Transcriptional regulation of Hepatic Stellate Cell activation in NASH
Non-alcoholic steatohepatitis (NASH) is a growing cause of chronic liver disease, cirrhosis, and hepatocellular carcinoma. Hepatic fibrosis resulting from accumulation of extracellular matrix proteins secreted by hepatic myofibroblasts plays an important role in disease progression. Activated hepatic stellate cells (HSCs) have been identified as the primary source of myofibroblasts in animal models of hepatotoxic liver injury; however, so far HSC activation and plasticity have not been thoroughly investigated in the context of NASH-related fibrogenesis. Bioinformatic interrogation of the promoter sequences of activated genes combined with loss-of-function experiments indicates that the transcriptional regulators ETS1 and RUNX1 act as drivers of NASH-associated HSC plasticity. Taken together, our results implicate HSC activation and transcriptional plasticity as key aspects of NASH pathophysiology.